Frequency of Portal Vein Obstruction and Treatment Interventions Following Pediatric Liver Transplantation: A Single-Center Retrospective Review
Arielle Melen1, Leandra Bitterfeld2, Jorge Sanchez-Garcia3, Peter Feola4, Manuel Rodriguez-Davalos5, Catalina Jaramillo6.
1School of Medicine, University of Utah, Salt Lake City, UT, United States; 2Pediatric Solid Organ Transplant, Intermountain Health, Salt Lake City, UT, United States; 3Transplant Department, Primary Children's Hospital, Salt Lake City, UT, United States; 4Intermountain Pediatric Imaging, Interventional Radiology, Primary Children's Hospital, Salt Lake City , UT, United States; 5Department of Surgery, University of Utah School of Medicine, Salt Lake City, UT, United States; 6Division of Pediatric Gastroenterology, Hepatology and Nutrition, University of Utah, Primary Children’s Hospital , Salt Lake City, UT, United States
PORTAL Registry .
Background
Portal vein complications (PVC) after liver transplantation may compromise patient and graft survival. Due to the rarity of PVC, risk factors are unclear and management strategies differ. This study aims to identify risk factors of PVC and describe management strategies in patients at Primary Children's Hospital.
Methods
This is a retrospective study of pediatric patients transplanted June 2002-May 2023. Data were collected for participation in the PORTAL registry. Retransplants were excluded.
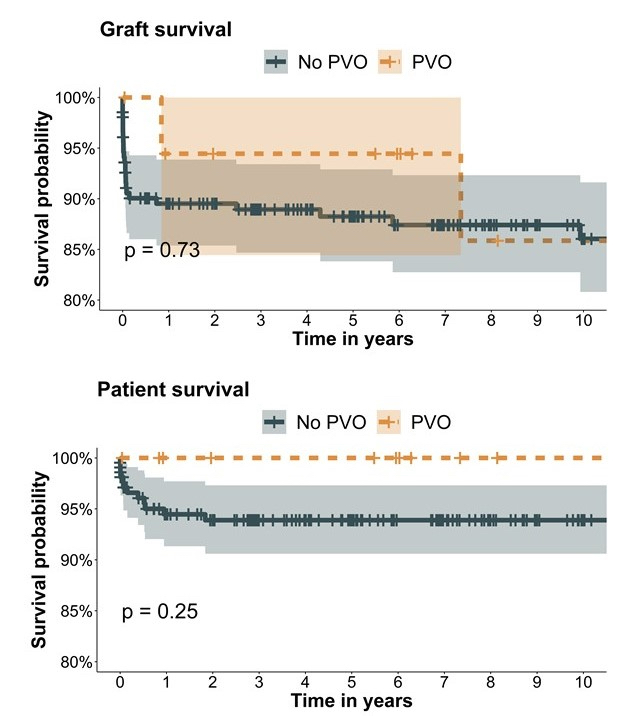
Children with and without PVC were compared using chi-square tests or T-tests. Risk factors were explored with multivariate regression models. Survival curves were compared by the log-rank test.
Results
PVC occurred in 19 of 235 (7.8%) children post-transplant. Children with PVC were younger (<1 year vs. 3 years, p<0.001) and smaller (7.4 kg vs. 14.5 kg, p<0.001) than those without PVC. There was no difference in donor type (deceased vs living; p=0.857) or transplant type (whole vs split; p=0.687). Children with PVC were hospitalized longer than those without PVC (28 days vs. 18 days p=0.002). When adjusting for transplant type, gender, and race/ethnicity, weight (OR:0.91; 95% CI:0.82-0.97, p=0.033) or age (OR:0.75; 95%CI:0.57-0.90, p=0.011) were significant in multivariate analysis. Graft (p=0.73) and patient (p=0.25) survival were similar.
The most common treatments for PVC were conservative treatment (n=10), surgical thrombectomy (n=8), and Meso-Rex bypass (n=3).
Conclusion
Smaller children are at higher risk of PVC. Despite variable management and longer hospitalizations, patient and graft survival are similar to patients without PVC. Limitations include the retrospective design, cohort heterogeneity, and low event frequency.
If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Sunday, October 15, 16:00-18:00 Monday, October 16, 07:00-18:00 Tuesday October 17, 07:00-12:30