A case of donor-derived syphilis seroconversion in a pediatric liver transplant recipient
Minoti Haribhai1, Elizabeth A Moulton2, Kristen G Valencia Deray2, Sarah K Nicholas3, Alison A Bertuch4, James J Dunn5, Flor M Munoz2, Anna M Banc-Husu1.
1Department of Pediatrics, Division of Gastroenterology, Hepatology, and Nutrition, Baylor College of Medicine, Texas Children's Hospital, Houston, TX, United States; 2Department of Pediatrics, Division of Infectious Diseases, Baylor College of Medicine, Texas Children's Hospital, Houston, TX, United States; 3Department of Pediatrics, Division of Allergy and Immunology, Baylor College of Medicine, Texas Children's Hospital, Houston, TX, United States; 4Department of Pediatrics, Division of Hematology and Oncology, Baylor College of Medicine, Texas Children's Hospital, Houston, TX, United States; 5Department of Pathology and Immunology, Baylor College of Medicine, Texas Children's Hospital, Houston, TX, United States
Introduction
Donor-derived syphilis is rarely reported. Given organ scarcity, syphilis is not a contraindication to donation. Donor-derived syphilis transmission has not been published to date in children undergoing liver transplantation (LT).
Case
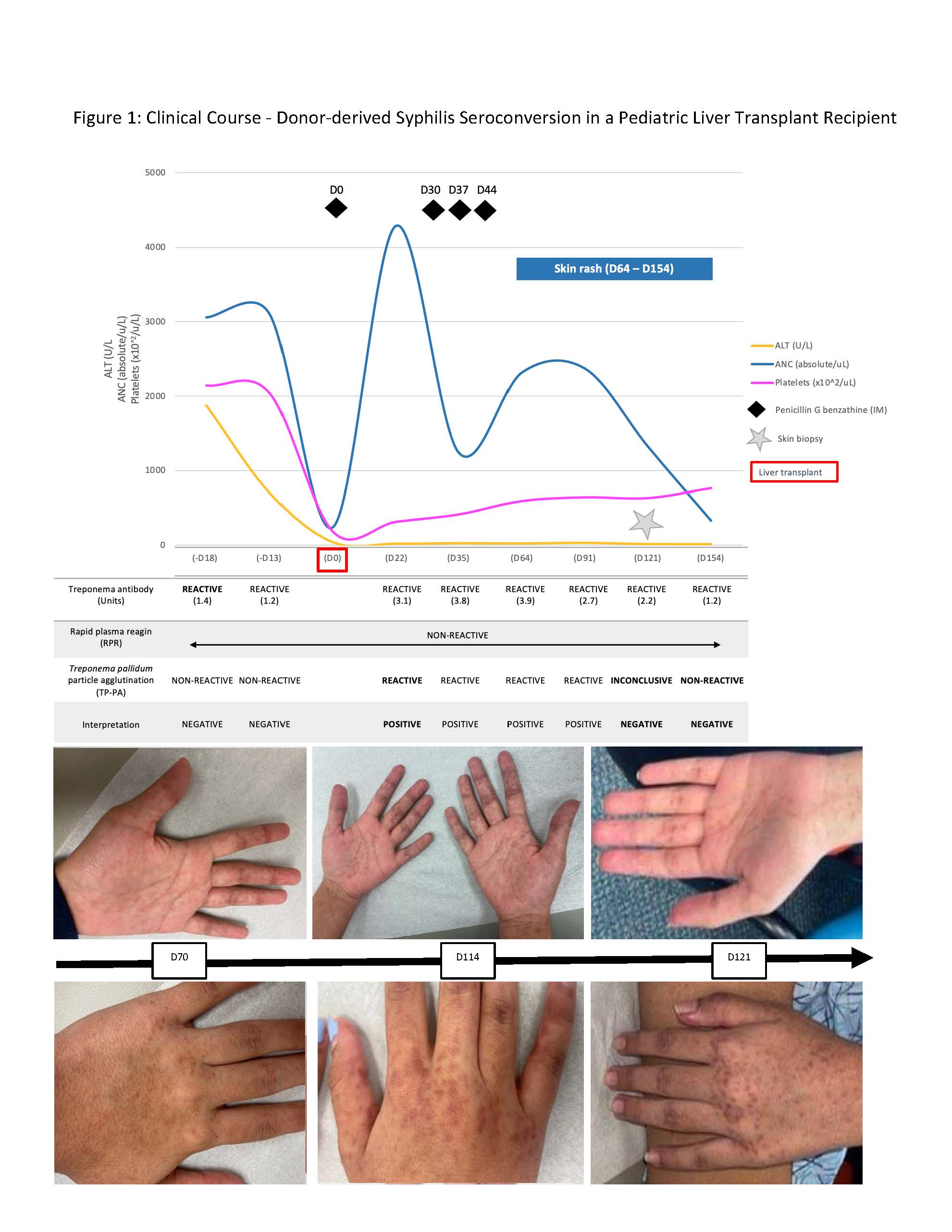
A previously healthy adolescent female with indeterminate acute liver failure underwent deceased-donor LT. The donor received penicillin for positive treponemal and non-treponemal syphilis testing (details unknown). Pre-transplant, recipient syphilis serologies were negative, and she received penicillin G benzathine (Pen-G) peri-operatively (Figure 1). She developed pancytopenia several days post-transplant, and bone marrow biopsy (D17) was suggestive of hepatitis-associated aplastic anemia. Repeat recipient syphilis testing was positive (D22); possible explanations included donor-derived infection, passive transfer of donor antibody, or transfer of antibody-producing donor B-lymphocytes. She received 3 weekly doses of Pen-G (D30, D37, D44). Around D64, she developed a maculopapular palmar and extremity rash reminiscent of secondary syphilis. Skin biopsy (D121) revealed perivascular dermatitis without other characteristic findings of syphilis or graft versus host disease (GVHD). Rash improved with topical steroids. On D154, TP-PA turned negative, suggesting positivity was due to donor antibody-producing B-lymphocytes that subsequently cleared. Chimerism testing revealed 55% donor T lymphocytes in blood (D161), raising concern for GVHD as the cause of rash and cytopenias.
Conclusion
To our knowledge, this is the first pediatric case of donor-derived syphilis seroconversion after LT, likely related to transfer of antibody-producing donor lymphocytes. This case highlights the challenge of interpreting recipient serological results when using syphilis-positive donors. Longitudinal studies examining syphilis seroconversion, therapy, and outcomes in this population are warranted.
If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Sunday, October 15, 16:00-18:00 Monday, October 16, 07:00-18:00 Tuesday October 17, 07:00-12:30