Immunologic tolerance after metachronous liver and bone marrow transplantation from different donors
Guillermo Costaguta1, Eytan Haddad2, Ludovic Civil2, Fernando Álvarez1,3, Mona Beaunoyer3,4, Pierre Teira3,5, Massimiliano Paganelli1,2,3.
1Gastroenterology, Hepatology and Nutrition, CHU Sainte-Justine, Montreal, QC, Canada; 2Liver Tissue Engineering and Cell Therapy, Research Center of the CHU Sainte-Justine, Montreal, QC, Canada; 3Department of Pediatrics, University of Montreal, Montreal, QC, Canada; 4Surgery, CHU Sainte-Justine, Montreal, QC, Canada; 5Hematology, CHU Sainte-Justine, Montrela, QC, Canada
Introduction: advances in the field of liver transplantation (LT) have caused an increase in the number of procedures performed each year. Lifelong immunosuppression is necessary, yet up to 30% of patients may develop tolerance. Bone marrow transplant (BMT) has been described after LT, but no publication has reported the use of a complete HLA mismatch between the liver and bone marrow allografts. We present the case of a liver transplant recipient who became immunotolerant after BMT.
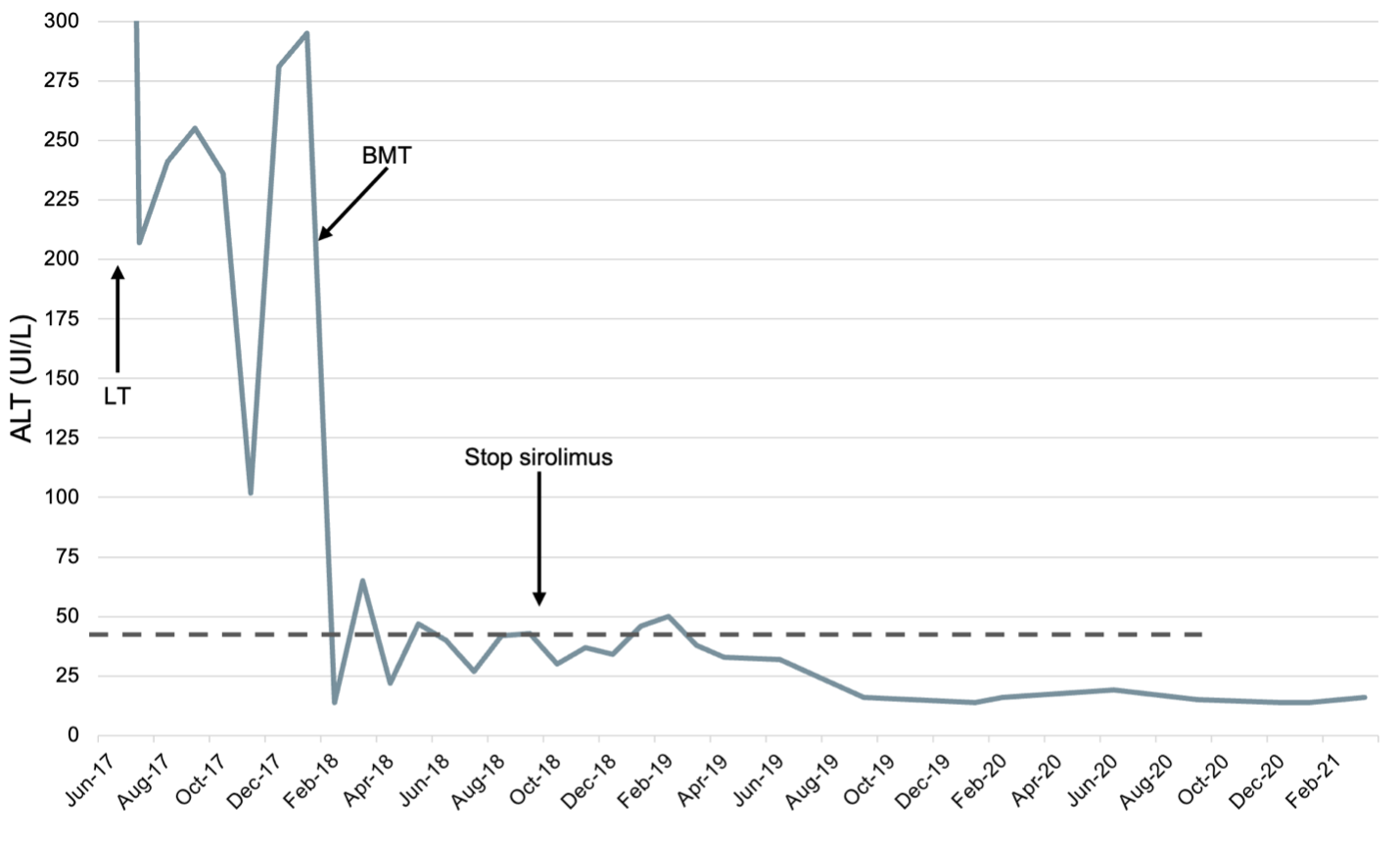
Case Report: a 14-year-old girl underwent LT for idiopathic subacute liver failure. Afterwards, she developed rapidly progressive pancytopenia. Liver function tests never normalised, and biopsies showed moderate cellular rejection despite multiple immunosuppressors (steroids, tacrolimus, mycophenolate, rituximab, and anti-thymoglobulin). Eight months after LT, BMT was performed for aplasia unresponsive to medical treatment. Despite 10/10 HLA match for the bone marrow, a complete mismatch (0/10) with the liver graft was noted. Immunosuppressors were stopped at BMT. Cyclophosphamide T-cell depletion and sirolimus monotherapy were chosen to improve the likelihood of tolerance. After BMT, improvement of liver function tests was noted with serial biopsies showing normalisation of histology. Six months later, sirolimus was weaned and stopped. Six years post-LT, she remains healthy, with normal liver function tests and free of immunosuppression.
Conclusion: this case shows that immunological tolerance after LT can be achieved with BMT and a tailored immunosuppression regimen. To our knowledge, this is the only case in the literature of tolerance, through BMT, despite a complete HLA mismatch between the liver and bone marrow allografts.
If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Sunday, October 15, 16:00-18:00 Monday, October 16, 07:00-18:00 Tuesday October 17, 07:00-12:30