Rise in the incidence of acute cellular rejection post-COVID: A large single center experience
Madelyn Cohen1, John A Goss2, Danielle Guffey3, Meghana Gudala3, Diana Harter3, Daniel Leung1.
1Department of Pediatrics, Division of Gastroenterology and Hepatology, Texas Children's Hospital, Baylor College of Medicine, Houston, TX, United States; 2Michael E. DeBakey Department of Surgery, Texas Children's Hospital, Baylor College of Medicine, Houston, TX, United States; 3Dan L. Duncan Institute for Clinical and Translational Research, Baylor College of Medicine, Houston, TX, United States
Introduction: Following the COVID-19 pandemic, in 2021-2022, we experienced an acute rise in the incidence of acute cellular rejection (ACR) episodes among children 1-year post liver transplant (LT) at Texas Children’s Hospital (TCH). We sought to identify clinical risk factors associated with this surge in ACR.
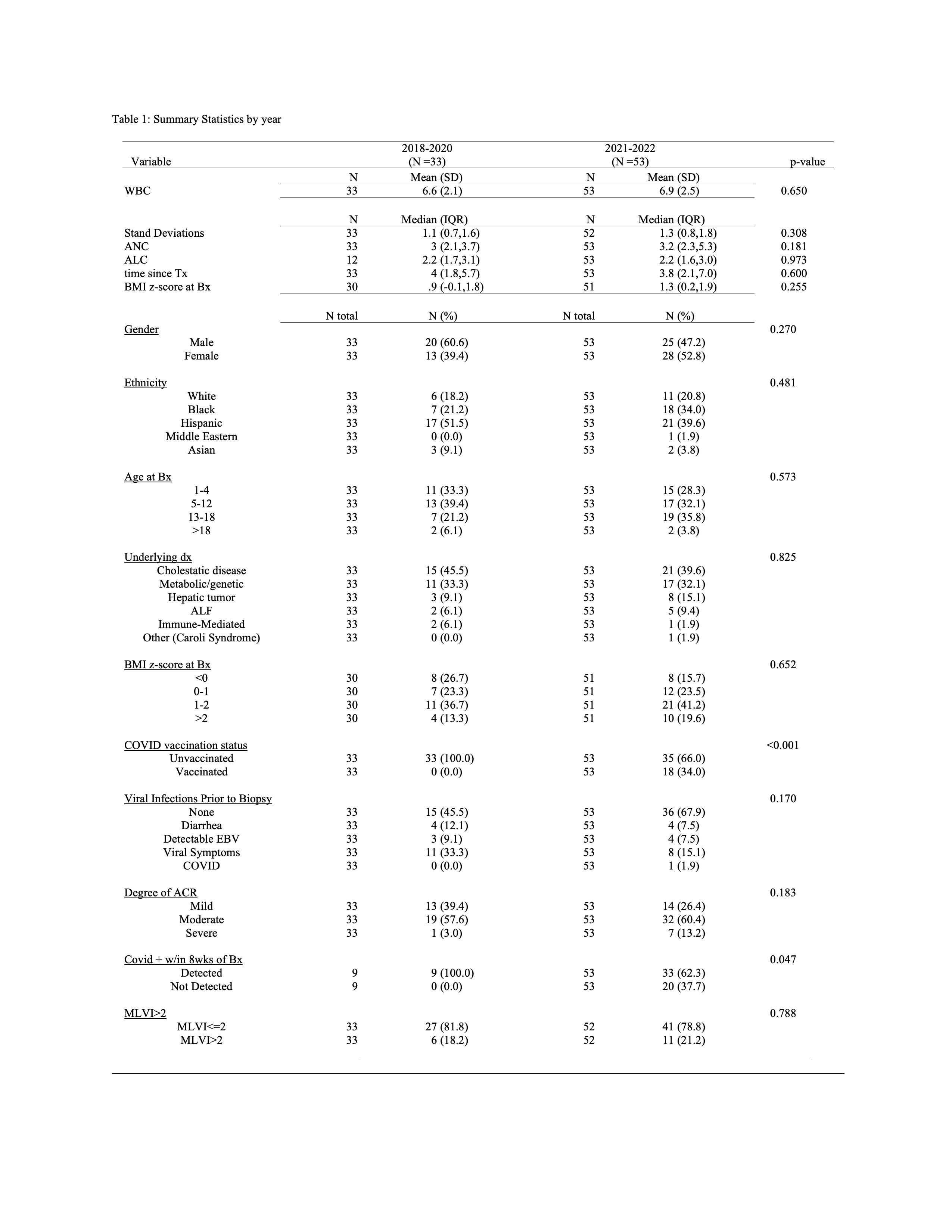
Methods: Baseline characteristics at or prior to time of histologically confirmed ACR were analyzed according to pre- (2018-2020) and post-COVID (2021-2022) eras using mean (SD), median (25th,75th %), or frequency (%). Unadjusted logistic regression assessed risk factors for ACR. All statistical analyses were performed using Stata v15.1.
Results: Among the 621 transplanted patients followed at our institution, 25 and 28 children were diagnosed with ACR in 2021 and 2022, respectively, representing a 2.2 and 2.5-fold increase compared to the 3 preceding years (n=11 per year, 2018-2020). Diagnosis, sex, ethnicity, and body mass index z-score were similar between eras. Post-COVID, there was a 50% increase in ACR among adolescents with a higher trend in severe ACR (RAI >6), but no differences in median MLVI. WBC, ALC and ANC were no different. Viral infections were less common (p=0.045), but not associated with increased ACR in the post-COVID era. COVID vaccination status in the higher ACR cohort mirrored the same proportion of the total transplant cohort (34%), suggesting that COVID vaccination status plays little or no role in the increased incidence of ACR.
Conclusion: Increased ACR rates at a large tertiary pediatric transplant center was not associated with viral infections, COVID vaccination, or increased MLVI.
If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Sunday, October 15, 16:00-18:00 Monday, October 16, 07:00-18:00 Tuesday October 17, 07:00-12:30