Invasive fungal infections (IFI) in children on liver transplant (LT) waitlist for initial or re-transplantation: A large single center experience
Madelyn Cohen1, Flor M Munoz2, Krupa R Mysore1.
1Department of Pediatrics, Division of Gastroenterology and Hepatology , Texas Children's Hospital, Baylor College of Medicine, Houston, TX, United States; 2Division of Infectious Diseases, Texas Children's Hospital, Baylor College of Medicine, Houston, TX, United States
Background: IFIs are associated with high morbidity and mortality in patients awaiting LT. Largely undefined in pediatrics, we aimed to assess the incidence, clinical manifestations, and outcomes of IFI in children listed for initial LT or retransplant.
Methods: Records of children listed for LT between January 2012 and December 2022 were reviewed for IFI, defined as histopathological evidence of fungal tissue invasion; isolation from blood culture, normally sterile body fluid or site; or imaging and clinical course consistent with IFI.
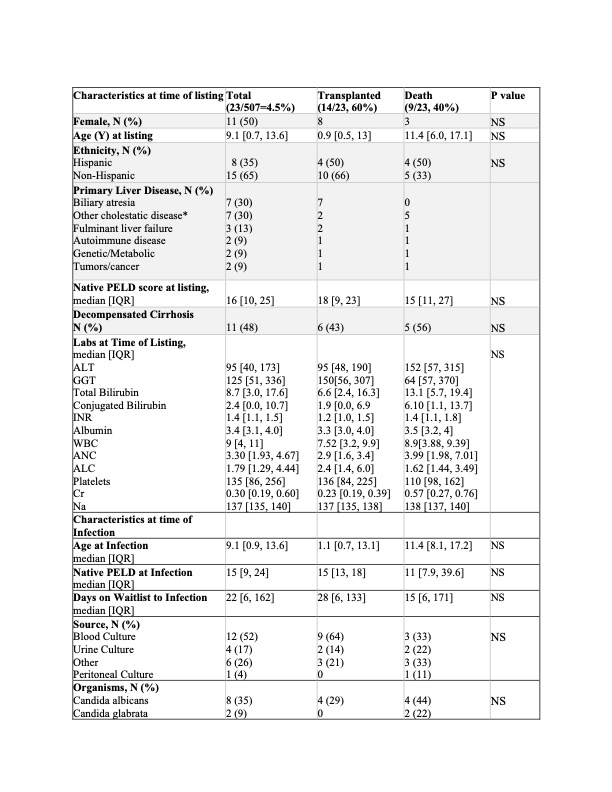
Results: 23/507 (4.5%) children listed for LT over 11-years had IFI; 9 (40%) children died. Patients who died were older (mean age: 11 years, IQR: 6.0, 17, p=0.09) than survivors, with a shorter median time from listing to IFI (15 days, IQR: 6, 171, p=0.28). Median time from infection to death was 11 days [IQR:10, 23]. There were no significant differences in listing indications, decompensated cirrhosis, or laboratory values at listing. Incidence of bacterial and viral infections, immunosuppression, and antibiotic exposure within the one-month preceding IFI were also similar amongst groups. Fungemia was the most common type of infection. Conjugated bilirubin, ANC, ALC, Cr and CRP at time of infection were significantly higher among the patients that died.
Incidence of IFI was >3 fold higher (7/39, 18%) in children listed for re-transplant. Total and conjugated bilirubin at listing and ALT, total and conjugated bilirubin, WBC and ANC at IFI diagnosis were significantly higher in children with IFI listed for re-transplant. There was higher mortality in children with IFI listed for retransplant (6/7, 89%) compared to those with IFI during initial listing (p=0.305). Median time from infection to death in the children listed for re-transplant was 16 days [IQR: 5, 28]. Candida spp. were most common pathogen overall.
Conclusion: While IFI in children awaiting initial LT was uncommon, mortality was high. Children re-listed for LT had a higher IFI incidence and mortality. Studies are needed to identify and treat patients at risk for IFI given the high waitlist mortality.
If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Sunday, October 15, 16:00-18:00 Monday, October 16, 07:00-18:00 Tuesday October 17, 07:00-12:30